PTSD can turn ordinary moments into a minefield. Used with care, meditation for PTSD triggers can steady the nervous system within minutes, help you ride out surges of emotion, and—over time—bring symptoms down a notch. Women are roughly twice as likely to develop PTSD as men, which means a trauma‑informed approach isn’t optional for Millennial and Gen Z women seeking practical, science‑literate tools. After 2020, when mindfulness app downloads spiked during lockdowns (as The Guardian reported), many people discovered that breath and attention can be both medicine and—if misapplied—too much, too fast. My view: the method matters as much as the minutes.
Table of Contents
- Why meditation can help during triggers
- Safety first: trauma‑informed meditation
- A step‑by‑step plan: meditation for PTSD triggers
- Trauma‑informed meditation for PTSD triggers: practices to try
- When to seek more support
- Smart tips for consistency
- Image suggestion
- Bottom line
- Summary and CTA
- References
Why meditation can help during triggers
- It dampens hyperarousal. Slow, paced breathing nudges the body toward the parasympathetic “rest and digest” system. Reviews suggest breathing at roughly 4–6 breaths per minute boosts vagal tone and trims anxiety and heart rate. In plain terms: longer, slower exhales tell the body it’s safe enough to stand down.
- It builds attention control. Mindfulness trains the mind to notice a trigger, label it, and redirect attention—sometimes in seconds. That attentional “pivot” can interrupt a spiral before it takes the wheel. I’d argue this skill is the linchpin for coping in the real world.
- It can reduce symptoms. In a 2015 JAMA trial with veterans, mindfulness‑based stress reduction led to clinically meaningful improvement for 49% of participants, compared with 28% in an active control, alongside larger drops in symptom severity. A Harvard‑affiliated team has echoed similar patterns in anxiety and stress studies. Numbers aren’t everything, but these are not trivial effects.
Safety first: trauma‑informed meditation
Meditation for PTSD triggers must be built around safety. Some survivors feel worse with eyes‑closed stillness. Adverse experiences during meditation—dissociation, panic, grief surges—are documented in the literature, so adapt the practice rather than push through it.
- Choose your posture and gaze. Sit or stand. Keep your eyes open, softly focused on a neutral spot. Lights on, door visible.
- Short beats long. Use 30–90‑second “micro‑practices” when triggered; extend to 3–10 minutes only when you’re steady.
- Keep control. You decide when to pause or stop. If distress climbs, pivot to grounding that orients you to the here‑and‑now.
- Work with support. A therapist trained in trauma‑informed meditation can calibrate practices to your window of tolerance. Evidence‑based trauma therapies remain first‑line; meditation is an adjunct, not a substitute. That boundary protects outcomes.
A step‑by‑step plan: meditation for PTSD triggers
1) Name it and orient
- Silently label: “I’m triggered; I’m safe enough right now.”
- Turn your head and eyes; identify three real‑time cues of safety—today’s date, a familiar object, a recent supportive text. Naming specifics matters.
2) Regulate with breathing exercises for PTSD
- Pursed‑lip breathing: Inhale 3–4 counts, exhale 6–8. Longer exhales cue downshift.
- Box breathing: Inhale 4, hold 4, exhale 4, hold 4—repeat 4 cycles. Military and clinical settings use this for a reason.
- Straw breath: Inhale through the nose, exhale slowly through pursed lips as if through a straw for 60–120 seconds. If dizziness appears, soften the effort.
3) Ground in the senses
- 5–4–3–2–1: Name 5 things you see, 4 you feel, 3 you hear, 2 you smell, 1 you taste. Out loud if possible.
- Temperature reset: Hold something cool; note precise sensations for one minute—edges, texture, temperature. I find temperature shifts cut through mental noise.
These grounding techniques tether you to the present when emotions swell.
4) Gentle focus meditation
- Anchor: Choose a neutral anchor—breath, contact at the feet, or a steady sound. For 1–3 minutes, rest attention there; when the mind jumps to the trigger, note “remembering” or “worry,” then return. Brief, light, repeatable.
- Set a floor: Keep roughly 70% of awareness on the anchor, 30% on the rest of experience. That way, you don’t get flooded by either the practice or the memory.
5) Self‑compassion check‑in
- Hand on heart. Inhale: “This is hard.” Exhale: “I’m here for me.” Short compassion cues can lower shame and reactivity; for many, this is the missing piece. It’s small, but not soft.
6) Debrief and plan
- Rate distress 0–10 before and after. If it didn’t drop by at least 2 points, shorten sessions, add more grounding, or involve a therapist.
- Schedule 2–3 brief reps daily when you’re not triggered; skill grows between storms. Consistency beats intensity.
Trauma‑informed meditation for PTSD triggers: practices to try
Orienting + breath (90 seconds)
- Look around and name the colors in the room—out loud if you can.
- Inhale 3, exhale 6 for 8 slow breaths.
Counting sounds (2 minutes)
- Eyes open. Count 10 distinct sounds—near, then far. If a memory intrudes, label “past,” return to the next sound.
Feet‑first body scan (2–4 minutes)
- Place attention on the soles of the feet, then calves, then hips. Skip the torso if it feels loaded. Stop if dissociation rises; that’s data, not failure.
Mantra focus (2 minutes)
- Silently repeat a neutral phrase such as “Right now, this breath.” Repeated‑word practices have shown PTSD symptom reductions in veteran samples. Neutral language can work better than affirmations during acute stress.
When to seek more support
- If meditation for PTSD triggers regularly spikes panic, dissociation, or self‑harm urges.
- If nightmares, avoidance, or hypervigilance persist beyond a month.
- Ask about trauma‑focused therapies—prolonged exposure, cognitive processing therapy, EMDR. Current VA/DoD guidance lists these as first‑line; mindfulness can complement them, not compete.
Smart tips for consistency
- Pair with routines: 60 seconds before opening messages or after brushing teeth. Habit stacking works.
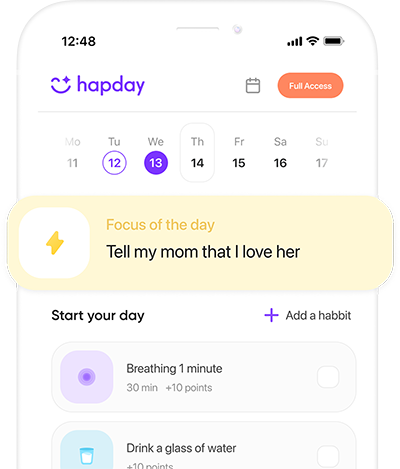
- Use tech: Set a timer paced to 4–6 breaths/min; choose trauma‑informed apps with open‑eye options and emergency stops.
- Track patterns: Which grounding methods lower your distress fastest? Keep a brief log; two weeks of notes often reveal your best levers.
Image suggestion
A sunlit, uncluttered corner—woman sitting upright, eyes open, one hand on heart, one on thigh. Alt: woman practicing meditation for PTSD triggers in a calm room.
Bottom line
Done gently and on your terms, meditation for PTSD triggers can move the body out of threat mode, strengthen attention control, and soften shame. Begin with breathing exercises for PTSD, layer in sensory grounding, and keep the frame trauma‑informed. If symptoms persist, pair these tools with therapy; that combination gives the best odds.
Summary and CTA
Meditation for PTSD triggers works best when it’s short, flexible, and safety‑focused. Blend paced breathing, open‑eye focus, and sensory grounding; track what reliably lowers distress. Evidence suggests mindfulness can reduce PTSD symptoms, but trauma‑focused therapy is the gold standard. Start small, practice between triggers, and get support if you’re stuck.
Start your first 90‑second plan today and share it with a trusted friend.
References
- Polusny MA et al. Mindfulness‑based stress reduction for PTSD in veterans. JAMA. 2015. https://pubmed.ncbi.nlm.nih.gov/26161861/
- Zaccaro A et al. How breath‑control affects physiology and attention. Front Hum Neurosci. 2018. https://pubmed.ncbi.nlm.nih.gov/29904372/
- Lindahl JR et al. Adverse meditation experiences. PLoS One. 2017. https://pubmed.ncbi.nlm.nih.gov/28542454/
- Kessler RC et al. Prevalence and correlates of DSM‑IV disorders (NCS‑R). Arch Gen Psychiatry. 2005. https://pubmed.ncbi.nlm.nih.gov/15699226/
- VA/DoD Clinical Practice Guideline for PTSD (2023). https://www.healthquality.va.gov/guidelines/MH/ptsd/