If you’re healing from trauma, connection can feel complicated—bracing one minute, comforting the next. Yet it’s also a powerful buffer against symptoms. This guide shows how to use 7 Love Languages for PTSD in a practical, consent-first way. Research has repeatedly linked social support with lower PTSD severity and better recovery odds; NIMH’s own figures show women experience PTSD at nearly twice the rate of men, a disparity that still deserves more daylight. I’ve seen, again and again, that steady support outperforms grand gestures.
Table of contents
- Before you start: consent and safety
- Words of Affirmation: using 7 Love Languages for PTSD
- Quality Time: structuring 7 Love Languages for PTSD
- Acts of Service: practical 7 Love Languages for PTSD
- Gifts: gentle 7 Love Languages for PTSD
- Physical Touch: trauma-wise 7 Love Languages for PTSD
- Shared Experiences/Play: playful 7 Love Languages for PTSD
- Digital Connection: modern 7 Love Languages for PTSD
- Evidence snapshot to anchor your plan
- Putting it together: a weekly micro-plan
- Red flags
- Bottom line
- Summary
- References
Before you start: consent and safety
- Ask-first rule: “Would this feel supportive right now?” It’s the non-negotiable.
- Go slow: aim for calm, not intensity—slow is often faster in trauma work.
- Agree on a pause word. Stopping on a dime is a sign of care, not failure.
- Therapy is core; use 7 Love Languages for PTSD as a supplement, not a substitute. When in doubt, defer to your clinician.
Words of Affirmation: using 7 Love Languages for PTSD
Why it helps: Shame and self-blame are frequent companions to PTSD; brief, believable statements can soften both. A 2012 synthesis on self-compassion found links to lower anxiety and depression, which tracks with clinical experience. I’m convinced the right sentence, offered at the right moment, can do more than an hour of advice.
Try this:
- To your partner/friend: “I believe you. Your reactions make sense.”
- Self-affirmation: Write 3 statements daily that validate your effort, not outcomes: “I am allowed to heal at my pace.”
- Crisis cards: Create a notes app list of grounding affirmations for flashbacks.
Quality Time: structuring 7 Love Languages for PTSD
Why it helps: Consistent, predictable presence reduces hypervigilance. Social connection buffers stress reactivity and can reduce symptom flare-ups; the effect shows up across meta-analyses and in living rooms. Predictable beats dramatic—almost always.
Try this:
- Co-regulate: Schedule a 10–15-minute “quiet time” together—no problem-solving, just breathing, tea, or a simple walk.
- Predictability pact: Share calendars for routines (sleep, meals, therapy) to reduce uncertainty triggers.
- Micro-dates: Low-stimulus activities (puzzles, knitting, plant care) that don’t overwhelm.
Acts of Service: practical 7 Love Languages for PTSD
Why it helps: Executive function and energy can dip with PTSD; triaging chores and logistics keeps life from tilting into chaos. There’s nothing trivial about clean dishes when your nervous system is on high alert. I’d argue this is the most underrated love language in recovery.
Try this:
- Triage tasks: Choose one 10-minute job together (dishes, laundry, insurance call) to keep chaos from snowballing.
- Aftercare: Prep a post-therapy kit—snack, water, weighted blanket, playlist.
- Sleep guardrail: Teammate handles bedtime routine (lights, screens, sound machine) to protect sleep, which is critical in PTSD.
Gifts: gentle 7 Love Languages for PTSD
Why it helps: Small, intentional items can cue safety, grounding, and self-soothing. Think sensory anchors over surprises. Thoughtful, not expensive, wins—every time.
Try this:
- Grounding kit: Smooth stone, lavender sachet, peppermint gum, stress ball, soft socks.
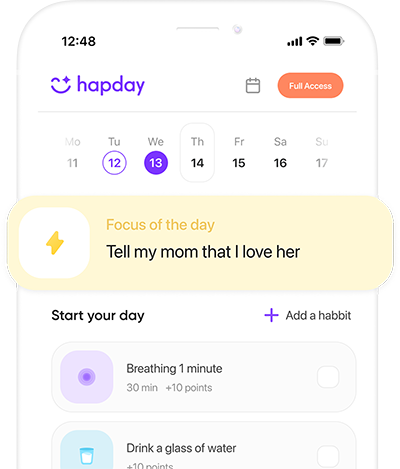
- Comfort subscriptions: Tea sampler, guided journaling, or mindfulness app gift codes.
- Memory-safe gifts: Avoid surprises if they trigger; share what’s inside first.
Physical Touch: trauma-wise 7 Love Languages for PTSD
Why it helps: Affectionate contact can reduce blood pressure and support oxytocin release, which may calm stress circuits. Consent and pacing are the whole ballgame. In my view, any touch without choice erodes trust, however “loving” it looks.
Try this:
- Touch menu: Create options rated 1–5 for intensity (hand squeeze, back-of-hand touch, handholding, head rub, hug). Update often.
- Touch scripts: “Hand on your shoulder for 10 seconds?” “Stop?”
- Self-touch: Butterfly hug (crossed arms, gentle alternating taps) during distress.
Shared Experiences/Play: playful 7 Love Languages for PTSD
Why it helps: Positive novelty nudges the nervous system toward safety, joy, and flexibility. Movement is a known modulator of arousal—small doses count. Play is not frivolous; it’s medicine with better branding.
Try this:
- Low-stakes novelty: Daytime museum, beginner class, scenic bus ride, nature trail.
- Movement snacks: 5–10 minutes of yoga, walking, or dancing—shown to help PTSD symptoms.
- Joy jar: Write tiny adventures on slips; pick one weekly.
Digital Connection: modern 7 Love Languages for PTSD
Why it helps: For many, text and voice notes feel safer than in-person processing and provide rapid support. During 2020–2021, telehealth use surged; the comfort of asynchronous care didn’t vanish when clinics reopened. I’d take a steady voice note over a rushed call any day.
Try this:
- Check-in ladder: Send 1) green/yellow/red emoji to share state; 2) a need emoji (ear, heart, tool).
- “Save for later” note: Drop hard topics in a shared doc to discuss when regulated.
- Asynchronous care: Voice note with breathing count-in (inhale 4, exhale 6) for grounding.
Evidence snapshot to anchor your plan
- Prevalence: Roughly 3.6% of U.S. adults have PTSD in a given year; lifetime risk is about 6.8%, with women at higher risk (NIMH; Kessler et al., 2005). Numbers are dry, but they counter the “it’s just me” lie.
- Social support: Across meta-analyses, stronger support tracks with less severe PTSD symptoms and better recovery—buffering that shows up then the stakes are highest.
- Touch and connection: Warm partner contact correlates with lower blood pressure and higher oxytocin (Grewen et al., 2005). More frequent hugs were linked to fewer infections and milder illness during high stress (Cohen et al., 2015), hinting at stress-buffering benefits.
- Exercise: Adding physical activity reduces symptom severity and improves mood for many (Rosenbaum et al., 2015). A brisk 10-minute walk is not nothing—it’s a nervous-system nudge.
- Self-compassion: Higher self-compassion is associated with lower psychopathology symptoms (MacBeth & Gumley, 2012), supporting the use of gentle affirmations and kind self-talk. Harvard-affiliated researchers have echoed these patterns in recent reviews.
Putting it together: a weekly micro-plan
- Pick 3 languages for this week. Choose for fit, not novelty.
- Set two tiny actions per language (under 10 minutes each). If it’s repeatable, it’s useful.
- Debrief gently: What felt good? Neutral? Too much? A few words are enough.
- Adjust intensity, never urgency. The point of using 7 Love Languages for PTSD is steady, predictable safety—let it do it’s job.
Red flags
- If touch, surprises, or intense talks spike dissociation or panic, scale way down and prioritize grounding. Your body is the data.
- If symptoms worsen or you feel unsafe, contact your clinician or crisis resources. Using 7 Love Languages for PTSD is an adjunct—not a replacement—for evidence-based care. As The Guardian reported during the pandemic, early outreach often prevents crises later.
[Image alt: How to Use 7 Love Languages for PTSD — calm couple journaling on a couch]
Bottom line
Relationships can be medicine when they are predictable, consent-based, and gentle. Using 7 Love Languages for PTSD helps you translate care into nervous-system safety. Start small, measure by calm rather then intensity, and let your plan evolve with your healing. Keep anchoring back to why you’re doing this: fewer spikes, more moments that feel like you.
Summary
Summary: With consent-first steps across words, time, service, gifts, touch, play, and digital care, you can use 7 Love Languages for PTSD to reduce arousal, increase safety cues, and steadily reclaim joy. Pair these micro-practices with therapy for best results. Bold move next: pick one action and schedule it today.
CTA: Save this guide, share it with your support person, and choose your first 10-minute step now.
References
- NIMH. Post-Traumatic Stress Disorder.
- Kessler RC et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders. Arch Gen Psychiatry. 2005.
- Brewin CR et al. Meta-analysis of risk factors for PTSD in trauma-exposed adults. J Consult Clin Psychol. 2000.
- Ozer EJ et al. Predictors of PTSD symptoms in adults: a meta-analysis. Psychol Bull. 2003.
- Grewen KM et al. Warm partner contact associated with oxytocin and lower BP. Psychosom Med. 2005.
- Cohen S et al. Hugging and social support protect against infection. Psychol Sci. 2015.
- Rosenbaum S et al. Exercise as treatment for PTSD: systematic review/meta-analysis. J Affect Disord. 2015.
- MacBeth A, Gumley A. Exploring self-compassion and psychopathology: a meta-analysis. Clin Psychol Rev. 2012.
- Coan JA et al. Handholding attenuates neural response to threat. Psychol Sci. 2006.