Table of Contents
- Introduction
- Why Meditation Helps During Panic
- How to Calm Panic Attacks with Meditation: A 5-Minute Plan
- Mindfulness for Anxiety: What the Science Says
- How to Calm Panic Attacks with Meditation While Commuting
- Build a Daily Practice to Calm Panic Attacks with Meditation
- Stickier Tips for Real Life
- Safety Notes
- Closing Thoughts
- Summary
- References
Introduction
If your heart is pounding, chest tight, and thoughts skittering in all directions, you’re not alone—and you can learn how to calm panic attacks with meditation. The National Institute of Mental Health estimates roughly 2.7% of U.S. adults meet criteria for panic disorder in a given year, with women reporting higher rates than men (3.8% vs. 1.6%). Eight weeks. That’s the time frame repeatedly shown in trials where mindfulness training reduces anxiety symptoms—not magic, just method. And in my view, a portable method is exactly what most people need.
[Image alt: woman practicing breathwork at home, how to calm panic attacks with meditation]
Why Meditation Helps During Panic
- Panic runs on a loop: a jolt of bodily sensation, the brain flags danger, adrenaline spikes—then the body reads that spike as proof of danger. Meditation trains attention to witness sensations as information rather than alarms. Simple idea; hard in the moment. Worth it.
- In randomized trials, mindfulness-based programs deliver moderate reductions in anxiety (effect size around 0.38, JAMA Intern Med). Slow, exhale-led breathing—a staple of panic attack breathing techniques—nudges the nervous system toward parasympathetic balance. Clinicians often target about six breaths per minute to support vagal tone and heart-rate variability.
- In patients with anxiety disorders (panic included), an 8-week mindfulness course performed as well as the medication escitalopram on a clinician-rated scale, with roughly a 30% drop in severity (JAMA Psychiatry, 2022). Noninferior isn’t a headline, but it’s meaningful.
How to Calm Panic Attacks with Meditation: A 5-Minute Plan
When a wave hits, try this micro-practice. It’s a guided meditation for panic attacks you can memorize and use anywhere—even standing in a grocery line.
- 1) Name it to tame it (10 seconds)
Silently label: “This is a panic attack. My body is safe, and this will pass.” Clear, firm language helps the prefrontal cortex re-engage and dials down amygdala overdrive. I’ve seen this simple line soften the sharpest edges. - 2) Orient to the room (30–45 seconds)
Turn your head gently. Identify 5 things you see, 4 you feel, 3 you hear, 2 you smell, 1 you taste. If numbers slip, no problem—stay with the senses. Anchoring to the present interrupts threat-fueled scanning. - 3) Exhale-led breathing (2–3 minutes)
- Inhale through the nose for 4.
- Exhale through the mouth for 6–8.
- Keep the breath low and quiet. Place a hand on your belly to feel it rise and fall.
Aim for ~6 breaths per minute. These panic attack breathing techniques bolster heart-rate variability and reduce sympathetic arousal. If you feel lightheaded, shorten the exhale slightly and soften the effort.
- 4) Feel, don’t fight (60 seconds)
Scan gently: where is the strongest sensation? Warmth in the face? Tightness in the chest or throat? Say: “Allow.” Give the sensation 10–20 seconds of space. Notice how it surges, plateaus, and shifts… even a 5% change matters. - 5) Re-engage one value
Ask, “What small action aligns with who I want to be?” Text a friend, sip water, or step outside for air. Meditation isn’t only stillness; it’s choosing your next helpful action on purpose. That’s the skill I’d bet on.
Mindfulness for Anxiety: What the Science Says
- A large review found mindfulness training improves anxiety and depressive symptoms compared with usual care, with benefits on par with established behavioral therapies (JAMA Intern Med, 2014). For a low-risk, low-cost tool, that’s a solid return.
- In panic-focused trials, mindfulness-based stress reduction and related programs lowered attack frequency and distress at rates similar to applied relaxation—and improved quality of life measures. Not flashy, but durable.
- Breathing is physiology, not platitude. People with panic often hyperventilate, lowering CO2 and amplifying symptoms (tingling, dizziness, chest tightness). Interventions that coach slower, steadier breathing can normalize CO2 over time and reduce attacks. A 2018 review in Frontiers in Human Neuroscience mapped these effects in detail.
How to Calm Panic Attacks with Meditation While Commuting
- Eyes open. Soften your gaze on a steady spot.
- Use 4–6 exhale-led breathing for 2–3 minutes.
- Count exhales up to 10; if you lose track, restart at 1 without judgment.
- Pair breath with movement: inhale as you step, exhale for two steps.
- If safe, use a short guided meditation for panic attacks in one earbud at low volume. During 2020, The Guardian reported meditation app use surged; commuters turned these practices into daily routines.
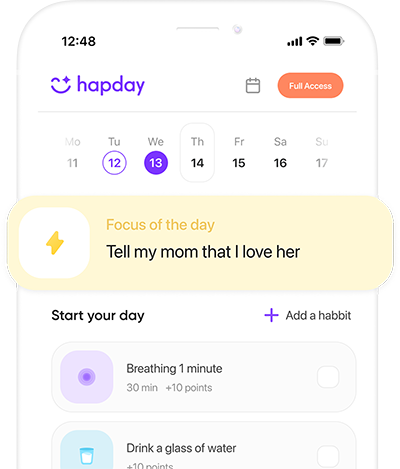
Build a Daily Practice to Calm Panic Attacks with Meditation
Consistency trains the nervous system between storms—when it’s most malleable.
- 10 minutes daily: Sit comfortably. Follow the breath. When the mind wanders, return kindly. This core mindfulness for anxiety builds attentional control and reduces reactivity. On restless days, two five-minute sits beat zero.
- Body scan (once/day): Sweep attention from toes to head, observing sensations without fixing them. Ideal pre-sleep; the body often follows the mind’s quieter lead.
- Loving-kindness (2–3 times/week): Repeat phrases like “May I be safe. May I be calm.” Compassion counters fear-based narratives, and—opinion here—it often softens shame, which keeps many people stuck.
- Weekly longer session (20–30 minutes): Use a guided meditation for panic attacks from reputable apps or university programs. Back in 2021, several academic centers expanded free libraries; they’re still there.
Stickier Tips for Real Life
- Pair practice with cues you already do (morning coffee, commute). Habit science favors anchors over willpower.
- Track: After practice, 0–10 rate anxiety and urge to avoid. Watch trends week to week, not hour to hour.
- Nudge physiology: Cool the face (splash water or rest a cold pack on cheeks/eyes). Brief facial cooling can stimulate the dive reflex and slow heart rate.
- Caffeine audit: High intake can mimic panic symptoms. Try a two-week reduction and log changes—you might learn more from that log than any blog.
- Therapy synergy: Combining mindfulness with CBT often accelerates gains by targeting both thoughts and body. Many clinicians now weave them together.
Safety Notes
- If you have asthma, cardiac issues, or feel worse with breath holds, skip holds and simply lengthen exhales gently.
- If panic is frequent, disabling, or accompanied by suicidal thoughts, reach out to a professional. In the U.S., call or text 988 for immediate support; for chest pain or signs of heart attack, call emergency services. Panic is common; its impact is not a character flaw.
Closing Thoughts
Learning how to calm panic attacks with meditation is a trainable skill. You practice when nothing is on fire so that, under pressure, the body recognizes a route home. With exhale-led breathing, mindful attention, and brief guided practice, you can interrupt the fear loop and recover faster. Start small, practice daily, and carry these panic attack breathing techniques and mindfulness for anxiety like a pocket toolkit—especially during spikes.
Summary
With solid evidence behind it, a brief, consistent practice—orienting, slow exhale breathing, and non-judgmental awareness—can ease panic quickly and build long-term resilience. Use a guided meditation for panic attacks when you need structure, and keep sessions short but daily. Bold step: schedule a 10-minute practice today. Bold CTA: Start your first 10-minute session tonight—set a timer now.
References
- National Institute of Mental Health (NIMH). Panic Disorder. https://www.nimh.nih.gov/health/statistics/panic-disorder
- Goyal M, et al. Meditation programs for psychological stress and well-being: a systematic review and meta-analysis. JAMA Intern Med. 2014;174(3):357-368. https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/1809754
- Hoge EA, et al. Mindfulness-Based Stress Reduction vs Escitalopram for the Treatment of Anxiety Disorders. JAMA Psychiatry. 2022;79(1):13-21. https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2798519
- Koszycki D, et al. Mindfulness-based stress reduction in generalized anxiety disorder and panic disorder: a randomized controlled trial. J Clin Psychiatry. 2007;68(7):936-945. https://pubmed.ncbi.nlm.nih.gov/17685713/
- Zaccaro A, et al. How breath-control can change your life: a systematic review on psycho-physiological correlates of slow breathing. Front Hum Neurosci. 2018;12:353. https://www.frontiersin.org/articles/10.3389/fnhum.2018.00353/full
- Meuret AE, et al. Respiratory and cognitive mediators of treatment change in panic disorder. J Consult Clin Psychol. 2008;76(5):695–708. https://pubmed.ncbi.nlm.nih.gov/18837588/